- HUMAN Diagnostics Worldwide
- Lab Professionals
- Trends & Topics
Supporting faster triage of COVID-19 patients by the use of hematology and CRP
In many countries, health organizations fear that they will find themselves in a situation where too many patients seek help in clinics, similar to the COVID 19 outbreak in Wuhan/China.
In order to cope with this situation in Wuhan, “fever” clinics were set up for patients with symptoms of infections. Typically, clinical manifestations of an infection are fever, fatigue and dry cough. Especially in the early stage of infection patients can be afebrile (without fever), with only chills and respiratory symptoms.
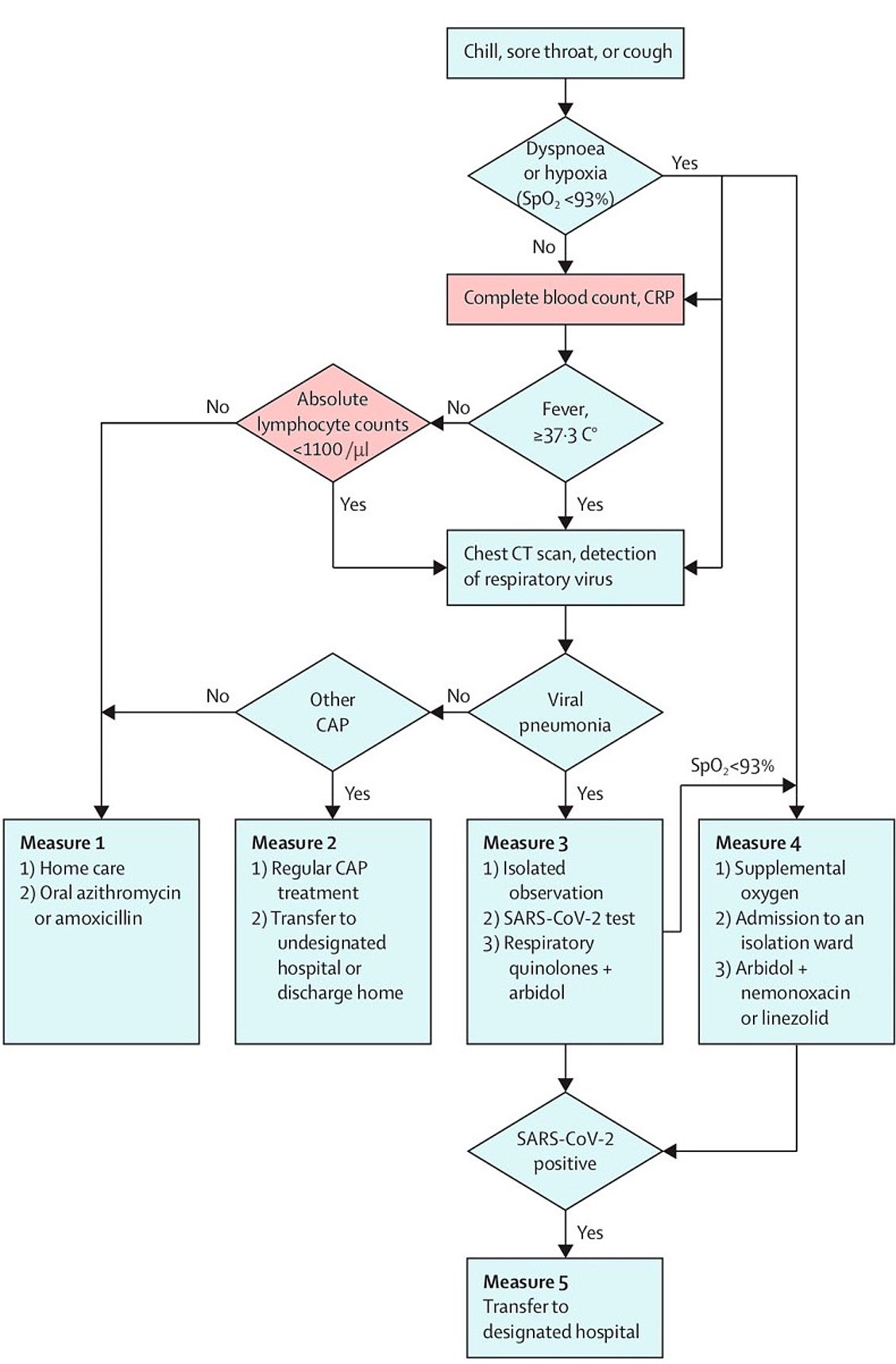
A recent publication by Lancet Respiratory Medicine describes the algorithm used to triage COVID-19 patients.1 Besides peripheral capillary oxygen saturation (SpO2), two other parameters played a central role: a lymphocyte count below 1100 /μl and an elevated CRP value. These parameters, in combination with the clinical signs, were used to differentiate patients requiring hospitalization from those who could stay at home with self-isolation.
Also other publications2,3 support the findings concerning lymphocytes and CRP of Zhang et.al.1. Chen et al. conclude:“In terms of laboratory tests, the absolute value of lymphocytes in most patients was reduced. This result suggests that 2019-nCoV might mainly act on lymphocytes, especially T lymphocytes, as does SARS-CoV. Damage to T lymphocytes might be an important factor leading to exacerbations of patients. The low absolute value of lymphocytes could be used as a reference index in the diagnosis of new corona virus infections in the clinic.”
Possibly, the observed low lymphocyte count is an indicator of immune suppression caused by the corona virus, similar to HIV infection for the CD4 count. CRP, often an indicator of bacterial infection, is also elevated in COVID-19 patients due to the viral infection. In critical patients, CRP levels rise continuously during the course of the disease.4
The Robert Koch Institute in Germany recommends regular determination of a differential blood count and CRP for monitoring the course of the disease.5 Also other countries are seeing hematology and CRP as essential parameters in the context of diagnosis and therapy decisions of COVID-19 patients.6
Literature
1. Jinnong Zhang, Luqian Zhou, Yuqiong Yang, et al. Therapeutic and triage strategies for 2019 novel coronavirus disease in fever clinics. Lancet Vol 8 March 2020. Doi: 10.1016/S2213-2600(20)30071-0
2. Chen et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395: 507–13. Doi:10.1016/S0140-6736(20)30211-7
3. Zhou et al. CT Features of Coronavirus Disease 2019 (COVID-19) Pneumonia in 62 Patients in Wuhan, China.Am J Roentgenol. 2020 Mar 05
4. Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7); Released by National Health Commission & State Administration of Traditional Chinese Medicine on March 3,2020
5. Torsten Feldt et al. Hinweise zu Erkennung, Diagnostik und Therapie von Patienten mit COVID-19; April 28, 2021; DOI: 10.25646/6539.226.
6. emcrit.org/ibcc/COVID19/; Possible diagnostic approach to ill patient admitted to hospital with suspected COVID-19
Flow chart for treatment of 2019 novel coronavirus disease in fever clinics in Wuhan China
Triage strategy according to Zhang et al.1
CRP=C-reactive protein.
CAP=Community-acquired pneumonia.
SARS-CoV-2=severe acute respiratory syndrome corona virus 2.