- HUMAN Diagnostics Worldwide
- Lab Professionals
- Trends & Topics
Rapid detection of cardiac troponin to help diagnose myocardial infarction
Imagine you are a physician or a paramedic called to an emergency. The patient presents with acute chest pain, shortness of breath, maybe nausea. It looks like a heart attack, but it can also be acute heart failure, cocaine abuse, something as banal as indigestion, or else.1 Perhaps you can record an electrocardiogram on site to help you differentiate, perhaps you cannot. What you know is that in the case of a heart attack “time is muscle and time wasted is muscle lost”!2 By intervening promptly you can save the patient’s life and limit the amount of damage to his or her heart.3 Luckily, you have a kit of troponin rapid tests at hand. You prick the patient’s finger, apply a bit of blood to the device and yes, you see the test line appear within minutes telling you that with high probability this is a heart attack. You can start managing the patient for adequate treatment immediately.
Figure 1. Cardiac troponin is the preferred diagnostic marker for heart attack. Rapid tests for cardiac troponin can be effective in helping to diagnose a heart attack earlier than central laboratories. (The structural illustrations of the cardiac troponin complex in the figure have been derived from the 1J1D crystal structure deposited at the RCSB PDB.4, 5
Heart attack
A heart attack (myocardial infarction or MI) is a serious emergency that requires immediate medical attention.1 Most heart attacks happen suddenly when one of the arteries leading to the heart becomes blocked, usually by a blood clot, and cuts off the blood flow. A lack of blood restricts the supply of oxygen and nutrients. Without these, the cells of the heart start to die. That is why every second counts when it comes to heart attack treatment. An extensive blockage, especially in a major blood vessel, can cause a large heart attack. A large heart attack that is not treated early can lead to heart failure, a life-threatening condition. Coronary artery disease - a build-up over time of plaque from fat and other substances that makes the arteries grow narrower or harder - is most often at the root of MI.
Rapid diagnosis of heart attack is critical for early treatment
The extent of permanent damage to the heart resulting from occlusion of a coronary artery can largely be avoided by timely reperfusion therapy. Reperfusion therapy includes drugs and surgery. The drugs applied to counter MI dissolve the clot blocking the artery. Blood flow can also be restored surgically by opening up the artery at the clogged site (coronary angioplasty) or grafting a new artery around the blockage (coronary bypass).6
Rapid diagnosis of acute MI is critical for early treatment. Unfortunately, the typical symptoms associated with MI - acute chest pain often accompanied with pain in the upper body, shortness of breath, nausea, tiredness, sweating – are not necessarily present in each case, nor are they unique to this condition.7 The clinical assessment, even when combined with an electrocardiogram (ECG), is thus often not sufficient to diagnose or exclude MI. Blood tests to measure the concentration of cardiac troponin (cTn) form the cornerstone for the early diagnosis of MI.8
Cardiac troponins as diagnostic markers of heart damage
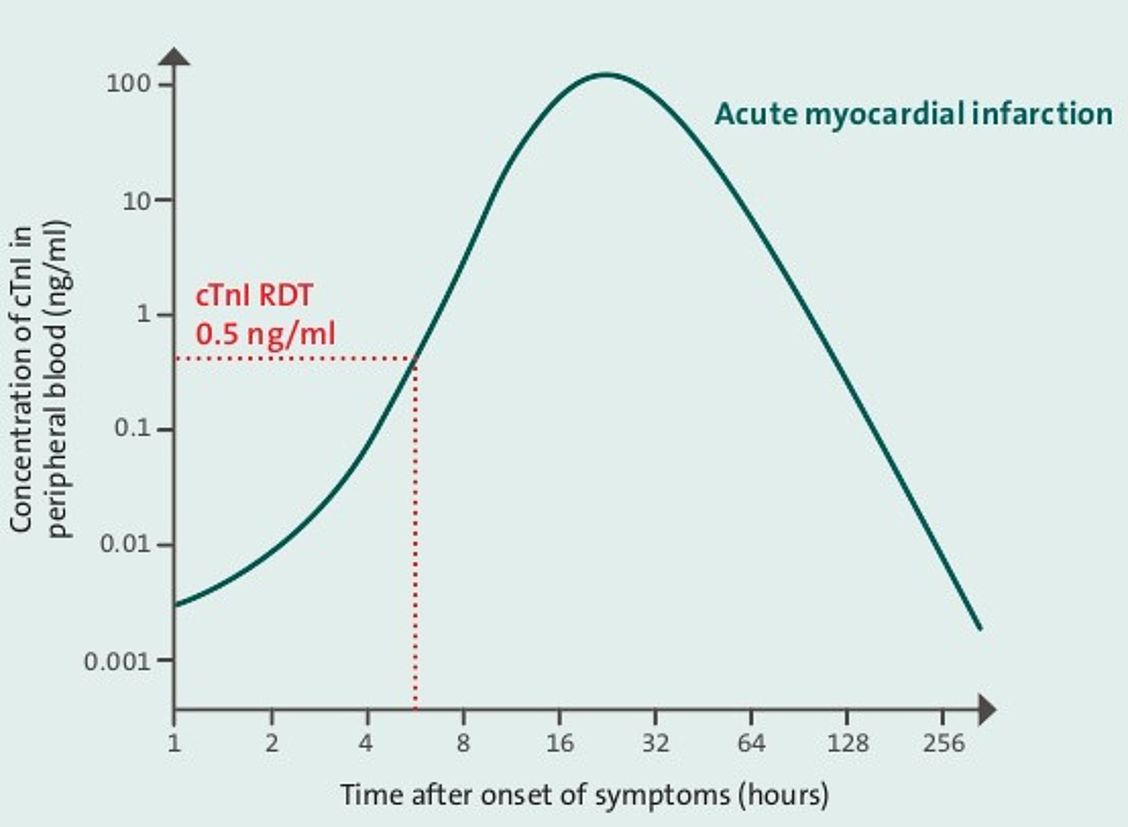
Troponin is a regulatory protein complex involved in the functionality of muscle cells. It is composed of three subunits: Troponin I, T and C (cTnI, cTnT and cTnC, respectively).9 Heart muscle cells express isoforms of cTnI and cTnT that are structurally distinct from their skeletal counterparts. Cardiac and skeletal isoforms of troponin C, on the contrary, are too similar to be distinguished by standard diagnostic methods. Levels of cTnI and cTnT in the blood are normally very low. Death of heart muscle cells (myocardial necrosis) results in the release of cTnI and cTnT into the bloodstream. The concentration of cardiac troponin (cTnI) in peripheral blood rises following a heart attack from the base level up to 100-fold. Immunoassays specific for the cardiac isoforms of troponin can detect a rise in their levels in peripheral blood regardless of the levels of skeletal troponins. Although a number of immunoassays specific for either cTnI or cTnT have been developed, they all meet the same performance specifications, and no distinction is made in terms of their diagnostic and prognostic utility. cTn (I or T) is the preferred biomarker of myocardial necrosis due to its superior performance in the diagnosis and prognosis of cardiac conditions.6 As cTnI assays are more common than cTnT assays, our discussion below will focus on cTnI.
Diagnostic testing for elevated cardiac troponin
Over the past decade cTnI assays have been improved regarding sensitivity. In our days, the diagnostic cut-offs for elevated cTnI of laboratory-based assays are in the range of 0.01-0.05 ng/ml. [10] Most rapid tests with visual readout have diagnostic cut-offs between 0.5 and 1 ng/ml (Hexagon Troponin: 0.5 ng/ml) which is higher than the cut-offs of laboratory-based assays. What are the benefits of a rapid test compared to a laboratory-based cTnI assay, then?
Rapid tests can help to rule-in MI earlier than laboratory-based assays
Clearly, there are reasons common to rapid diagnostic test (RDT) devices in general: ease of use, robustness, instrument-free readout and compatibility with capillary blood obtained by fingerstick. The key reason, however, is the RDT’s ability in certain settings to reveal elevated cTnI earlier than a laboratory-based assay. It holds for myocardial infarction that early treatment is critical to avoid extensive damage to the heart. Paramount to early specific treatment of MI is early diagnosis. An RDT can be used to rule-in MI whenever it can deliver the result earlier than an alternative assay.
Under what circumstances is the use of a rapid test for troponin particularly beneficial?
Prehospital diagnosis
One typical scenario where a cTnI RDT can support rule-in of MI faster than a central laboratory is that of first contact of paramedics with an emergency patient. The level of cTnI in peripheral blood starts to rise gradually a few hours after MI and typically peaks 24-48 hours later at up to 100 times the baseline (Figure 2). Serious cases of MI or cases where several hours have passed from the onset of symptoms until contact with the emergency responders can already be identified on site or during transport to hospital. The patient can then be managed effectively by means of drugs during transport, by direct transfer to a hospital capable of adequate treatment, by arranging in advance for immediate cardiac imaging and coronary angioplasty in the receiving hospital, etc.
Figure 2. The concentration of cardiac troponin (cTnI) in peripheral blood rises following a heart attack from the base level up to 100-fold. The diagnostic cut-off for elevated cTnI is about 0.5 ng/ml for qualitative rapid diagnostic tests for cTnI (cTnI RDT). Figure adapted from Mahajan and Jarolin, Circulation, 2011.11
Remote settings
In remote settings often either no laboratory or only basic equipment is available. It can take hours to have a sample of the patient’s blood delivered to a central laboratory. Furthermore, a cTnI test on a laboratory-based assay is associated with a significant turnaround time. In stark contrast, a cTnI test with an RDT can be done on site and the result is available almost instantly. If positive, appropriate management of the patient can start immediately.
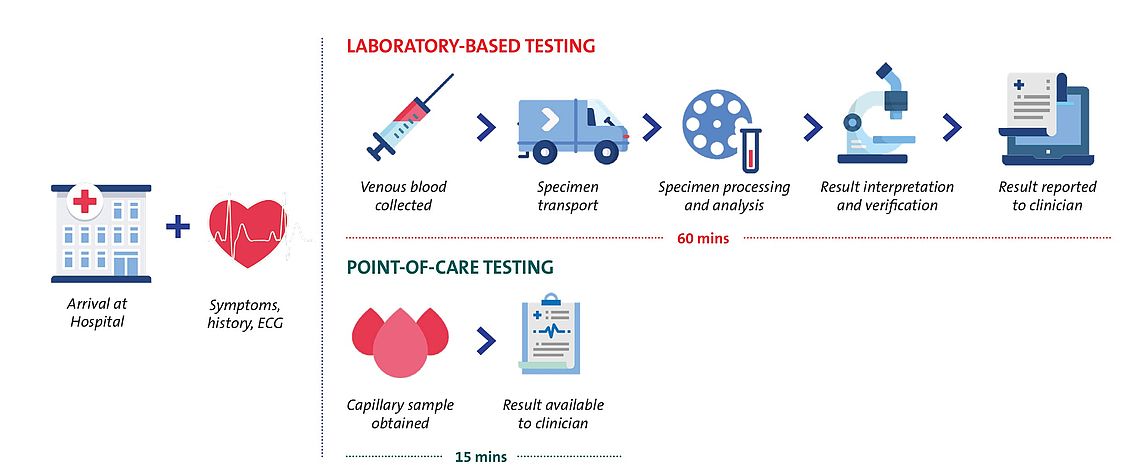
Overcrowded emergency department
Overcrowding in the emergency department (ED) of a hospital is a widely acknowledged problem that has been shown to result in increased inpatient death.12 Current guidelines of leading cardiological associations suggest that cTn results be made available to physicians within 60 minutes from ED arrival.13, 8 Contrary to these recommendations, even in developed countries the typical turnaround time (time from blood draw at the emergency department to result) for a cardiac troponin test in the ED is one to two hours.14 Overcrowding in the ED often leads to disruptions in sample processing and gives rise to still longer laboratory turnaround times.15 In contrast, a point-of-care test for cTn, such as with a cTnI RDT, is simple to perform by nursing staff in a manner independent of the central laboratory. By quickly identifying cases of highly elevated cTnI, the RDT can in a short time deliver crucial information for patient triage. This way it can not only improve the outcome for the particular patient by decreasing the delay to treatment, but also relieve the overall strain on the ED and the central laboratory.
Summary
Rapid tests for cTnI are easy to use and read, robust, compatible with capillary blood and, above all, fast. For these features, they are ideal to help diagnose myocardial infarction in prehospital or remote settings. cTnI RDTs can also be useful in triage in the emergency departments. Diagnosis of acute MI should not be based on the results of the rapid test only, however, but include patient symptoms and, if available, ECG and/or angiographic evidence. Rapid tests for cTnI allow for rule-in but not for rule-out of acute MI. Nevertheless, a consistently negative result with a qualitative rapid test for cTnI with serial blood draws in the time window of hours to days after onset of symptoms may indicate a milder form of MI or other heart disease.
Figure 3 Testing for cardiac troponin in patients with suspected heart attack at point of care compared with testing at central laboratory. Point-of-care testing may allow rule-in of myocardial infarction earlier than laboratory-based testing.16
References
| 1 | O. J. Mechanic and S. A. Grossman, Myocardial Infarction, Acute, StatPearls Publishing, 2018. |
| 2 | E. Braunwald, Evolution of the management of acute myocardial infarction: A 20th century saga, vol. 352, Elsevier Limited, 1998, pp. 1771-1774. |
| 3 | "Heart attack - your quick guide | BHF," [Online]. Available: www.bhf.org.uk/informationsupport/publications/heart-conditions/heart-attack---your-quick-guide. |
| 4 | S. Takeda, A. Yamashita, K. Maeda and Y. Maéda, "Structure of the core domain of human cardiac troponin in the Ca2+-saturated form," Nature, vol. 424, no. 6944, pp. 35-41, 3 7 2003. |
| 5 | "RCSB PDB - 1J1D: Crystal structure of the 46kDa domain of human cardiac troponin in the Ca2+ saturated form," [Online]. Available: www.rcsb.org/structure/1j1d. |
| 6 | K. Thygesen, J. S. Alpert, A. S. Jaffe, B. R. Chaitman, J. J. Bax, D. A. Morrow and H. D. White, "Fourth Universal Definition of Myocardial Infarction (2018)," Journal of the American College of Cardiology, vol. 72, no. 18, pp. 2231-2264, 30 10 2018. |
| 7 | R. Twerenbold, J. Boeddinghaus, T. Nestelberger, K. Wildi, M. Rubini Gimenez, P. Badertscher and C. Mueller, Clinical Use of High-Sensitivity Cardiac Troponin in Patients With Suspected Myocardial Infarction, vol. 70, Elsevier USA, 2017, pp. 996-1012. |
| 8 | M. Roffi, C. Patrono, J.-P. Collet, C. Mueller, M. Valgimigli, F. Andreotti, J. J. Bax, M. A. Borger, C. Brotons, D. P. Chew, B. Gencer, G. Hasenfuss, K. Kjeldsen and P. Lancellotti, "2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation," European Heart Journal, vol. 37, no. 3, p. 267–315, 2016. |
| 9 | "Troponin - StatPearls - NCBI Bookshelf," [Online]. Available: www.ncbi.nlm.nih.gov/books/NBK507805/. |
| 10 | F. S. Apple, Y. Sandoval, A. S. Jaffe and J. Ordonez-Llanos, "Cardiac Troponin Assays: Guide to Understanding Analytical Characteristics and Their Impact on Clinical Care," Clinical Chemistry, vol. 63, no. 1, pp. 73-81, 1 1 2017. |
| 11 | V. S. Mahajan and P. Jarolim, "How to interpret elevated cardiac troponin levels," Circulation, vol. 124, no. 21, pp. 2350-2354, 22 11 2011. |
| 12 | B. C. Sun, R. Y. Hsia, R. E. Weiss, D. Zingmond, L. J. Liang, W. Han, H. McCreath and S. M. Asch, "Effect of emergency department crowding on outcomes of admitted patients," Annals of Emergency Medicine, vol. 61, no. 6, p. 605, 2013. |
| 13 | A. H. B. Wu, R. H. Christenson, D. N. Greene, A. S. Jaffe, P. A. Kavsak, J. Ordonez-Llanos and F. S. Apple, "Clinical Laboratory Practice Recommendations for the Use of Cardiac Troponin in Acute Coronary Syndrome," Clinical Chemistry, vol. 64, no. 4, pp. 645-655, 1 4 2018. |
| 14 | C. Ho, K. Cimon, L. Weeks, M. Mierzwinski-Urban, L. Dunfield, L. Soril, F. Clement and M. Jabr, "Point-of-Care Troponin Testing in Patients With Symptoms Suggestive of Acute Coronary Syndrome: A Health Technology Assessment Economic authors:," A Health Technology Assessment, vol. 5, no. 1b, 2016. |
| 15 | K. D. Rooney and M. M. Schilling, "Point-of-care testing in the overcrowded emergency department - Can it make a difference?," Critical Care, vol. 18, no. 1, p. 692, 8 12 2014. |
| 16 | A. R. Chapman, S. Stewart and N. L. Mills, Contemporary point of care cardiac troponin testing in suspected acute coronary syndrome, vol. 105, BMJ Publishing Group, 2019, pp. 740-741. |