- HUMAN Diagnostics Worldwide
- Lab Professionals
- Trends & Topics
Procalcitonin (PCT) - Different PCT levels due to different pathogens
Procalcitonin is an important biomarker for bacterial infections and in particular for thediagnosis, monitoring and treatment surveillance of sepsis. Some interesting findings andrecent developments in the scientific community suggest that PCT may become evenmore valuable as a biomarker.

Since bacterial endotoxins trigger PCT production, is it possible that some bacterial infections do not show elevated PCT levels?
In some cases, PCT levels may not be elevated like one would expect with bacterial infections. The reasons for this observation can be manifold and it needs to be emphasized that the production of PCT can be triggered by endotoxins and inflammatory host cytokines.1
What exactly are endotoxins?
Endotoxins or lipopolysaccharides (LPS) are components of the outer cell membrane (OM = outer membrane) of Gram-negative bacteria. Endotoxins are released by living Gram-negative bacteria through the cleavage of vesicles (OMVs; Outer Membrane Vesicles), or when Gram-negative bacteria die. Examples of Gram-negative bacteria are of the group Enterobacteria, Pseudomonas, Legionella, Neisseria and Rickettsia. Therefore, Gram-negative bacteria should result in elevated PCT levels in severely ill patients.
What are the effects of bacterial endotoxins?
Endotoxins can produce fever when coming into contact with mucous membranes and pass into the blood. They also activate a number of signaling pathways of immunocompetent cells, which can lead either to inflammation or to programmed cell death (apoptosis) of these cells.
Do all Gram-negative bacteria express endotoxins?
No, there are exceptions. Some atypical bacteria, like the Gram-negative bacterium Mycoplasma pneumoniae, do not possess an outer cell membrane and therefore do not have endotoxins (LPS). Other atypical bacteria like the Gram-negative Chlamydia pneumonia with a low-level of endotoxin, may show patients with normal PCT levels. However, a study on children aged 2-14 years who were hospitalized for community-acquired lower respiratory tract infections (LRTIs) diagnosed acute Chlamydia pneumoniae infections in 14% and acute M. pneumoniae infections even in as high as almost 35%.2 Patients infected with above mentioned atypical bacteria usually have lower PCT levels that would not indicate antibiotic therapy.3 This nicely highlights that clinicians cannot rely on PCT alone to guide antibiotic treatment decisions but PCT levels are to be used in conjunction with other laboratory findings and the clinical assessment.
Do Gram-positive bacteria produce endotoxins?
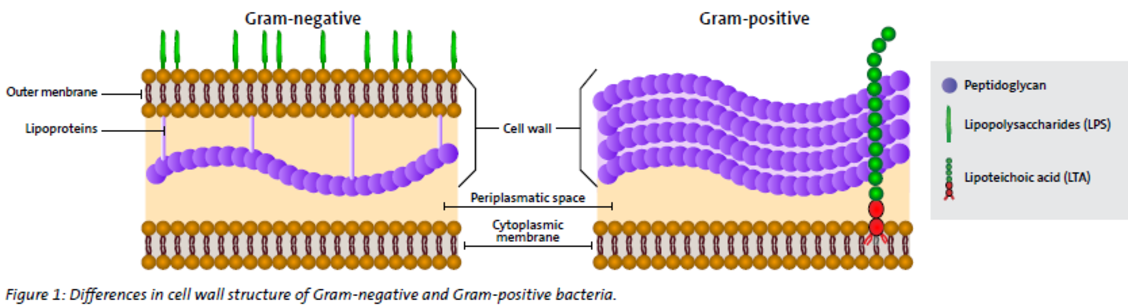
No, Gram-positive bacteria do not have an outer membrane containing endotoxins (LPS). Unlike Gram-negative bacteria that express endotoxins in their outer membrane, Gram-positive bacteria contain lipoteichoic acid (LTA) as the major component of their cell wall, instead (see figure 1). Examples of Gram-positive bacteria are of the group Streptococcus, Enterococcus, Staphylococcus, Listeria, Bacillus, and Clostridium. However, PCT levels in the blood of patients infected with Gram-positive bacteria are found to be elevated, as other pathogen associated molecular patterns (PAMPs) also trigger immune reactions.
If Gram-positive bacteria do not produce endotoxins, why then does the PCT concentration in the blood increase?
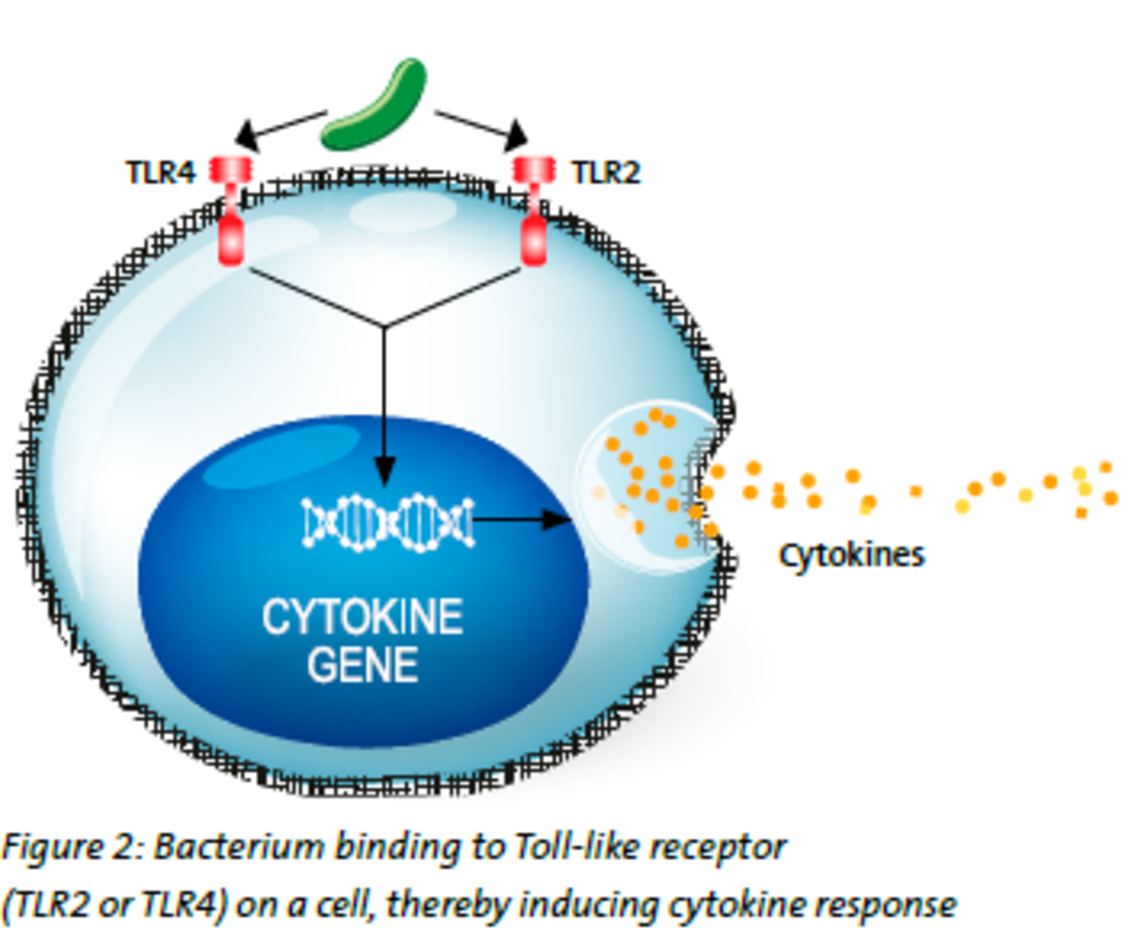
Procalcitonin (PCT) is produced in response not only to bacterial endotoxin, but also in response to inflammatory host cytokines.1 The underlying mechanism is still not completely clear. But it is known that lipoteichoic acid (LTA) that exists in the cell walls of Gram-positive, is recognized by a receptor, called Toll-like receptor 2 (TLR2), whereas lipopolysaccharides (LPS), that exist in the cell walls of Gram-negative bacteria, is recognized by a different receptor, namely Toll-like receptor 4 (TLR4).4 Patients infected with Gram-positive bacteria have elevated PCT levels, probably as a result of the response of inflammatory cytokines (see figure 2).
Is it possible to discriminate Gram-negative from Gram-positive bacteria with PCT?
Recent publications suggest that different pathogens could lead to different levels of PCT production. A recent study found that the PCT levels in Gram-negative bloodstream infections was significantly higher than those in Gram-positive bloodstream infections and fungal bloodstream infections.5 Although the exact mechanisms are not yet fully understood, the observed differences of PCT levels in response to different pathogens like Gram-positive, Gram-negative and fungi, may be partly due to the differences in pathogenic inflammatory signalling pathways and cytokines.4
Could PCT testing take antibiotic stewardship one step further?
The observed PCT level differences in relation to different pathogens could be of special relevance in bloodstream infections, in which PCT could assist clinicians in evaluating the more appropriate initial antimicrobial therapy. This could be especially valuable in those cases in which clinicians would need to wait for species identification in patients’ blood cultures for an additional 1 to 2 days.1
References
1. Leli C. et al. Procalcitonin levels in gram-positive, gram-negative, and fungal bloodstream infections. Dis Markers. 2015;2015:701480. doi: 10.1155/2015/701480. Epub 2015 Mar 17. PMID: 25852221; PMCID: PMC4380090
2. Principi N. et al. Role of Mycoplasma pneumoniae and Chlamydia pneumoniae in Children with Community-Acquired Lower Respiratory Tract Infections, Clinical Infectious Diseases, Volume 32, Issue 9, 1 May 2001, Pages 1281–1289, doi.org/10.1086/319981
3. Self W.H. et al. Procalcitonin as a Marker of Etiology in Adults Hospitalized With Community-Acquired Pneumonia. Clin Infect Dis. 2017 Jul 15;65(2):183-190. doi: 10.1093/cid/cix317. PMID: 28407054; PMCID: PMC5850442.
4. Wang D. et al.; The diagnostic ability of procalcitonin to differentiate Gram-negative bacteria from Gram-positive bacteria and fungal bloodstream infections in critically ill patients; European Journal of Inflammation; April 3, 2019; doi.org/10.1177/2058739219841469
5. Brodská, H. et al. Significantly higher procalcitonin levels could differentiate Gram-negative sepsis from Gram-positive and fungal sepsis. Clin Exp Med 13, 165–170 (2013). doi.org/10.1007/s10238-012-0191-81