- HUMAN Diagnostics Worldwide
- Lab Professionals
- Trends & Topics
Genetic characteristics influence susceptibility to COVID-19 Blood group A a risk factor for COVID-19?
The rapid global spread of the noval SARS-CoV-2 virus is straining existing health resources, so identifying infected persons and prioritising people at high risk has become a critical challenge.
Known risks
Clinical observations suggest that age, gender and certain chronic diseases (e.g. cardiovascular disease, lung disease, diabetes, hypertension) present a risk with SARS-CoV-2 and a higher disease severity.
Blood groups and genetic factors dependent risks
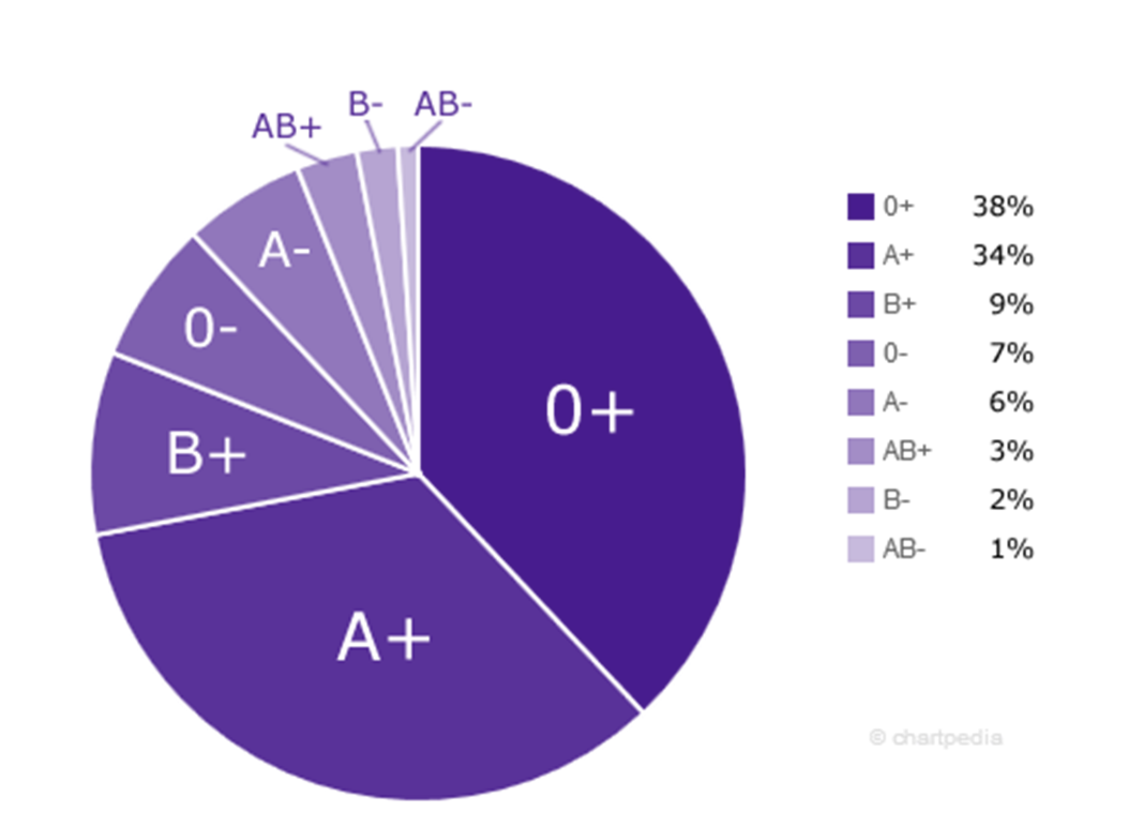
Novel studies show that the ABO blood groups could be biomarkers for the different susceptibility to COVID-19.1,2,3,5 The Chinese study1 concludes that blood group A is associated with an increased risk of SARS-CoV-2 infection and severe COVID-19, while blood group 0 is associated with a reduced risk compared to non-blood group 0. The American study2 concluded that the odds for positive COVID-19 test results is increased for blood group A and decreased for blood group 0. Due to the rare cases of rhesus negative blood, the result is only associated with rhesus positive blood groups. The figure below shows worldwide distribution of blood groups. In the third European study3, a genome-wide association analysis was performed with severe COVID-19 patients with respiratory failure from the the epicenters of the European pandemic. The researchers were able to identify gene variants on chromosomes 3 and 9 that were associated with severe COVID-19 courses. A strikingly large number of carriers of these two gene variants were people with blood group A. The data confirm that blood group A is associated with a higher risk than the non-A blood groups and the risk for blood group 0 is lower compared to the non-0 blood groups. People with blood group 0 seem to have a better immune defence against SARS-CoV-2 viruses and have the lowest risk of severe COVID-19 compared to blood groups A, B, AB. A conclusive explanation for the risk of the individual blood groups is currently lacking.
The results of these studies could lead to COVID-19 patients with blood group A being monitored more closely and treated earlier, and the identification of the two gene variants could help in the development of drugs against COVID-19.
Figure 1: Worldwide Distribution of Blood Groups4
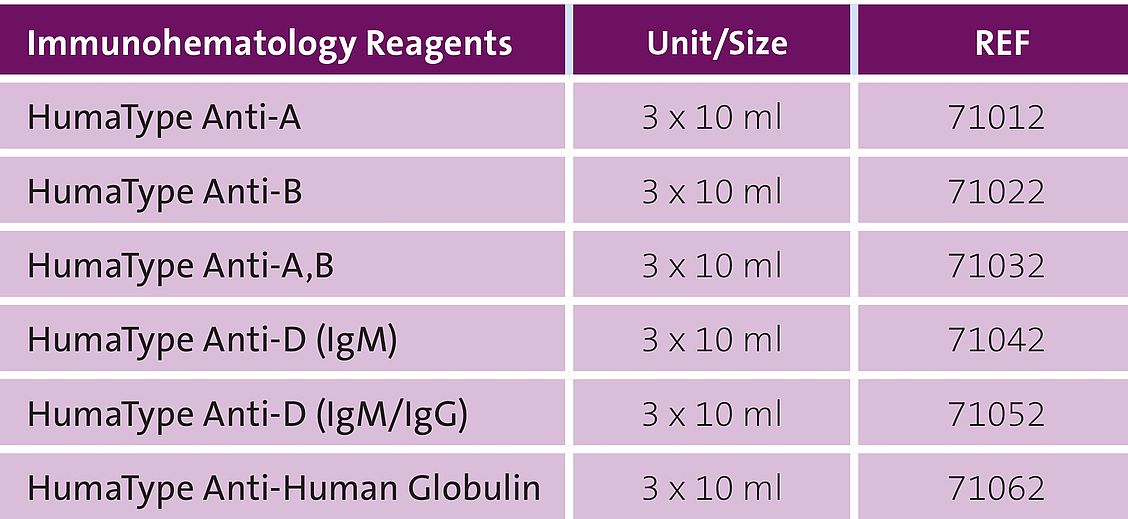
HUMAN HumaType reagent kits for blood group typing for manual procedures in tubes, on slides and plates
References
- Relationship between the ABO Blood Group and the Covid-19 Susceptibility, Jiao Zhao, et. al., medRxiv
- Testing the association between blood type and COVID-19 infection, intubation and death, Zietz, M. et. al., medRxiv
- Genomewide Association Study of Severe Covid-19 with Respiratory Failure, Ellinghaus, D et al., NEJM (2020)
- Chartpedia: de.chartpedia.org/img/blutgruppen-verteilung-weltweit.png, 20.07.2020
- The SARS-CoV-2 receptor-binding domain preferentially recognizes blood group A, Wu S-C. et al., Blood Adv (2021) 5 (5): 1305–1309.