- HUMAN Diagnostics Worldwide
- Lab Professionals
- Trends & Topics
PTH and 25-OH Vitamin D - The importance of calcium regulation in the body
Introduction on the importance of parathyroid hormone (PTH)
Recently, parathyroid hormone (PTH) immunoassay testing was added to the WHO 4th edition of the Essential IVD List (EDL) as an in vitro diagnostic tool (IVD) to aid in evaluating the causes of calcium homeostasis disorders and monitoring the effects of treatment.1

What is PTH?
Parathyroid hormone (PTH) is a hormone produced and released by the parathyroid glands, which are four tiny glands located behind the thyroid gland (see figure 1). PTH production is activated by low levels of calcium in the blood. PTH controls vitamin D levels, and both hormones — PTH and vitamin D —regulate calcium levels in the blood. Therefore, they are crucial factors in maintaining calcium concentrations at a normal level throughout the body. If the body has too much or too little PTH, it can influence the vitamin D level and cause symptoms related to abnormal blood calcium levels.2
Why test for PTH and vitamin D?
Abnormal blood calcium levels can cause serious health problems, like osteoporosis, rickets, or symptoms associated with hypercalcemia. As such, PTH and vitamin D are essential hormones that are central to maintaining the integrity and physiological function of the skeletal system, our body‘s largest organ.1
How do PTH, vitamin D, and calcium regulate each other?
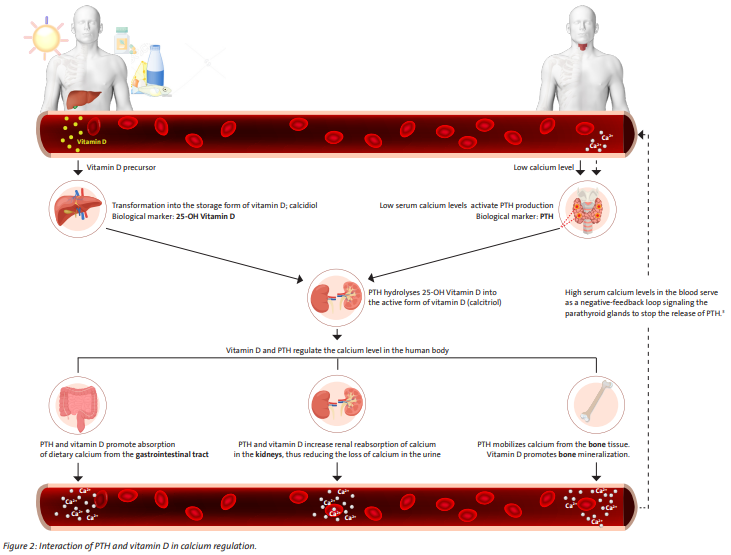
PTH levels are mainly controlled by a feedback loop from calcium levels to the parathyroid glands. In other words, when calcium levels are low in the blood, the glands are stimulated to release PTH into the bloodstream, whereas high calcium levels prevent the glands from releasing PTH. PTH, in turn, converts vitamin D into its active form in the kidneys.2
There are three main organs involved in the regulation of calcium levels by PTH and vitamin D (see figure 2). Both hormones increase calcium levels in the blood and support bone mineralization.
Kidneys
PTH and vitamin D increase calcium levels in the blood.
- PTH increases the renal tubular reabsorption of calcium ions back from urine.
- Vitamin D stimulates calcium reabsorption in the kidneys.
Intestins
PTH and vitamin D increase calcium levels in the blood.
- PTH increases enteral reabsorption of calcium ions.
- Vitamin D stimulates calcium reabsorption in the intestines.
Bones
PTH and vitamin D support the calcium homeostasis in the body.
- PTH mobilizes calcium ions from the bone tissue.
- Vitamin D promotes the mineralization of the bone.
The use of PTH and vitamin D blood testing in disease management
Low PTH levels
In hypoparathyroidism, the parathyroid glands do not respond with increased PTH secretion (which would be normal), although the serum calcium level is low. This malfunctioning of the parathyroid glands can occur due to an autoimmune attack on the parathyroid glands (which is common) or after thyroid surgery where the parathyroid glands have been partially removed (which is mainly the case).
The diagnosis involves PTH blood testing and monitoring of vitamin D supplementation.4
In hypercalcemia with advanced tumors, the parathyroid glands may release only a small amount of PTH because the blood contains too much calcium (hypercalcemia).
Hyperthyroidism can also cause elevated calcium levels, leading to decreased PTH levels in the blood. This is because severe hyperthyroidism accelerates bone metabolism, resulting in an increased release of calcium into the blood.
Vitamin D overdosage can be the cause of e.g. low PTH levels, potentially resulting in hypercalcemia.5, 12
Elevated PTH levels
Primary hyperparathyroidism (PHPT)
i.e., overactive parathyroid glands, mainly occurs due to benign growths (adenomas) and, less frequently, malignant growths (carcinomas), which can result in bone thinning because too much calcium is extracted from the bones. In some cases, PHPT can lead to kidney stones. The diagnosis includes PTH and vitamin D blood testing. 5, 6, 7

Secondary hyperparathyroidism
can be caused by constant stimulation of the parathyroid glands due to low calcium levels, leading to gland growth and hyperactivity (parathyroid hyperplasia), for example, in chronic kidney disease (CKD). This condition indicates the need for PTH blood testing to assess parathyroid function, estimate bone turnover, and guide therapy management.1, 8
Vitamin D deficiency
can also lead to secondary hyperparathyroidism, which must be differentiated from PHPT. Furthermore, the rates of nutritional rickets in children from developing countries have been estimated to be over 50%, representing a significant disease burden.1, 9
From the precursor to the active form of vitamin D
In the presence of sunlight (UV-B), a cholesterol precursor (7-dehydrocholesterol) in the skin is photochemically converted to vitamin D3. Vitamin D3 is also found in certain foods (e.g., fish, milk products) and is available as a dietary supplement. For vegans, mushrooms are an alternative. However, they contain the less bioavailable vitamin D2.
Both vitamins, D2 and D3, are converted in the liver into the storage form 25-OH vitamin D, which predominantly circulates in the blood. When thestorage form 25-OH vitamin D (calcidiol) reaches the kidneys, it is converted by parathyroid hormone (PTH) into the physiologically active form of vitamin D, called calcitriol, also known as 1,25(OH)2 vitamin D (see figure 4).
Biological marker 25-OH vitamin D
Vitamin D diagnostics detects the amount of 25-OH vitamin D in serum, providing information about vitamin D deficiency.
To be fully biologically active, 25-OH vitamin D needs to be converted to 1,25-dihydroxyvitamin D (1,25(OH)2 vitamin D) in the kidney cells. 25-OH vitamin D (the storage form of vitamin D) is the most suitable analyte for assessing vitamin supplies, D2 and D3, due to its low biological activity and its presence in high concentrations in the blood circulation.10
Vitamin D deficiency
Vitamin D deficiency occurs when the body‘s production is insufficient. The most common cause is a lack of exposure to sunlight, often compounded by a diet deficient in vitamin D. However, certain disorders can also lead to vitamin D deficiency. Insufficient vitamin D results in muscle and bone weakness and pain. In infants, it leads to rickets, while adults may suffer from osteoporosis. Because it is challenging to compensate for vitamin D deficiency through diet alone, supplementation is usually necessary.
Vitamin D overdose
An overdose of vitamin D can lead to coma. It is impossible to overdose on vitamin D through excessive exposure to sunlight or consuming foods rich in vitamin D, such as eggs, herring, and cheese. However, taking high doses of vitamin D supplements over a prolonged period is extremely dangerous: vitamin toxicity can lead to increased calcium concentration in the blood (hypercalcemia), causing calcium to accumulate in the blood vessels and kidneys. Elevated calcium levels can lead to a rapid decline in kidney function and cause conditions such as kidney stones and kidney failure. Those affected fall into a so-called hypercalcemic coma, which can be fatal.11
Summary of indications
PTH
- Aid in the differential diagnosis of primary hyperparathyroidism from other forms of hypercalcemia, hypocalcemia and parathyroid disorders.
- Monitoring patients with chronic kidney disease.
25-OH Vitamin D
- Aid in the assessment of Vitamin D sufficiency disorders.
- Monitoring of Vitamin D concentration levels.

References
1. WHO Technical Report Series 1053, The selection and use of essential in vitro diagnostics, Report of the fourth meeting of the WHO strategic Advisory Group of Experts on In Vitro Diagnostics, 2022 (including the fourth WHO model list of essential in vitro diagnostics), ISBN 978-92-4-008109-3 (electronic version)
2. https://my.clevelandclinic.org/health/articles/22355-parathyroid-hormone
3. Khan M, Jose A, Sharma S. Physiology, Parathyroid Hormone. 2022 Oct 29.
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 29763115
4. https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/hypoparathyroidism
5. https://www.apotheken-umschau.de/diagnose/laborwerte/parathormon-pth-erhoeht-den-blut-kalziumspiegel-742365.html
6. 1998-2023 Baylor College of Medicine, Healthcare: Endocrinology, Diabetes and Metabolism
7. https://www.niddk.nih.gov/health-information/endocrine-diseases/primary-hyperparathyroidism
8. https://columbiasurgery.org/conditions-and-treatments/secondary-hyperparathyroidism
9. N.Yedla, et.al., „Vitamin D Deficiency and the Presentation of Primary Hyperparathyroidism: A Mini Review“, International Journal of Endocrinology, vol. 2023, Article ID 1169249, 8 pages, 2023. https://doi.org/10.1155/2023/1169249
10. https://medlineplus.gov/lab-tests/vitamin-d-test/
11. https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/expert-answers/vitamin-d-toxicity/faq-20058108
12. Marcinowska-Suchowierska E, Kupisz-Urbańska M, Łukaszkiewicz J, Płudowski P, Jones G. Vitamin D Toxicity-A Clinical Perspective. Front Endocrinol (Lausanne). 2018 Sep 20;9:550. doi: 10.3389/fendo.2018.00550. PMID: 30294301; PMCID: PMC6158375.