- HUMAN Diagnostics Worldwide
- Lab Professionals
- Trends & Topics
Increased diagnostic efficiency by combining 5-Part differentiation and C-reactive protein.
Abstract
A fast turnaround time for diagnostic tests is important to enable healthcare professionals to quickly determine the appropriate treatment strategy for their patients at an early stage.
The combination of C-reactive protein (CRP) and complete blood count (CBC) parameters, typically included in early patient assessment, can reduce turnaround time and is beneficial for patients in medical practices, intensive care units, and emergency departments. This combination of parameters can be particularly beneficial in differentiating between bacterial and viral infections, but also plays a role in many other diagnostic areas such as fever investigations, acute and chronic inflammation, autoimmune diseases, Covid-19 infections, post-operative infection control and many more.
This article focuses on the benefits of combining CRP and CBC in one diagnostic system and how this can improve workflow and efficiency in diagnostics.
Complete blood count and C-reactive protein
A complete blood count (CBC) is an essential, comprehensive blood test that evaluates the type, number, size, and other characteristics of a patient's blood cells. The CBC measures the amount of red blood cells (RBC), platelets (PLT) and white blood cells (WBC) including the differential white blood count. Each of these types of blood cells performs important functions, so determining their levels can provide important information about general health and can help diagnose a number of health conditions.

It is an important medical tool because it uses a single sample to analyse the full range of cells found in the blood, as well as some of the physical characteristics of those cells1. A C-reactive protein test is often ordered along with a complete blood count. C-reactive protein (CRP) is a highly sensitive acute-phase protein that is released into the bloodstream within hours of injury, infection or other causes of inflammation.2,3
An increase in CRP levels may precede the clinical symptoms of a particular disease, such as pain or fever, which is useful for early diagnosis. CRP is particularly useful in the diagnosis and assessment of infections, fever investigations, differentiation between bacterial and viral infections and inflammatory conditions.
CRP and CBC are important diagnostic tools for a wide range of diseases and conditions.
Bacterial and viral infections cause similar symptoms such as weakness, fever, muscle aches and others. Currently, antibiotics are often freely prescribed without clinical confirmation of the presence of bacteria. Unfortunately, differentiating between bacterial and viral infections based on non-specific signs and symptoms can be difficult in many cases, such as respiratory infections.4,5,6
Early differentiation between the two types of infection is essential for appropriate treatment and prognosis. While bacterial infections are usually treated with antibiotics, antibiotic treatment of viral infections is ineffective and counterproductive. Inappropriate prescription rates and overuse of antibiotics have led to antimicrobial resistance, which is one of the greatest threats to global health.7 Therefore, antibiotics should only be prescribed and administered when needed according to current guidelines.8
The combination of a complete blood count and CRP is an effective way of improving diagnosis and can help reduce unnecessary use of antibiotics.9 The table below shows the CRP reference ranges for different pathological situations and possible causes:
|
CRP Range |
Disease activity |
Causes |
|
< 5 mg/L |
n. a. |
n. a. |
|
5 – 10 mg/L |
Low-grade inflammation |
Obesity, diabetes mellitus type 2, atherosclerotic cardiovascular diseases, smoking, pregnancy, etc. |
|
10 – 40 mg/L |
Mild inflammation |
Local abscess, minor surgical trauma, accidental trauma, myocardial infarction, deep vein thrombosis, inactive rheumatic disease, Crohn´s disease, metastatic malignant tumor, occasional viral infections etc. |
|
40 - 100 mg/L |
Moderate inflammation |
Severe inflammatory processes such as bronchitis, purulent cystitis, dental suppuration, urinary tract infection and genital infections. The infections require intervention, e.g., therapy with antibiotics. |
|
>100 mg/L |
High-grade inflammation |
Acute generalized infections caused by bacteria and fungi (sepsis), severe tissue damage after polytrauma or major surgical interventions |
(Adapted from: Thomas, L. C-reaktives Protein (CRP) In: Prof. Dr. Lothar Thomas, Kirschbaumweg 8, 60489 Frankfurt (ed.) Labor und Diagnose 2020. Chapter 19.4. Accessed September 19, 2023. https://www.labor-und-diagnose-2020.de)
While recent studies have highlighted newer biomarkers of bacterial infection, CRP and CBC remain cost-effective, with established laboratory standardization, including the availability of robust internal quality control (IQC) material and widely available external quality assurance (EQA) schemes. The literature reviewed suggests that, particularly in resource-limited settings, CRP testing may be beneficial in improving the rational use of antibiotics in febrile patients.10
Among other applications, the combination of a complete blood count and CRP plays an important role in the investigation of fevers such as malaria, dengue, etc. Although fever can be caused by a trivial infection, it can also be a manifestation of a rapidly progressing and fatal infection. A short time to diagnosis for early initiation of treatment may therefore be necessary to save a patient's life.11 The combination of a detailed review of the clinical course, physical examination, and laboratory data is crucial in determining the likely cause of the fever. For example, dengue and malaria infections, which often coexist in endemic areas, present with similar symptoms, and produce somewhat similar abnormalities in CBC parameters. The combination of CRP level and platelet (PLT) count can be useful in distinguishing between dengue and malaria, with a low PLT being indicative of dengue, whereas a low PLT count together with an elevated CRP level is more indicative of malaria.12 Many parasitic infections are associated with eosinophilia, but in malaria, which is a protozoan infection, EOS are within the normal range.13 CRP is not a specific biomarker for malaria and the sensitivity of CRP to viral infection is low. However, it is a useful parameter in understanding the etiology of infection and in distinguishing malaria and dengue fever from other diseases with similar hematological abnormalities.14 However, dengue and other non-viral infections can coexist in a single specimen, so relying on CRP alone should not be an exclusive criterion for differentiating between the two diseases.
|
Disease |
Type of infection |
WBC |
PLT |
EOS |
CRP |
|
Dengue fever |
Virus |
Very low |
Very low |
Normal/Low |
Normal |
|
Malaria |
Protozoa |
Normal/Low |
Low |
Normal/Low |
High |
Table 1: Findings in assessment of malaria and dengue patients
During the Covid-19 pandemic, CRP played an important role in the diagnosis and monitoring of the disease. At the beginning of the pandemic, when neither PCR nor rapid tests were available, there was a need to establish a practical and efficient way of screening large populations for Covid-19 infection. Early reports from China recommended that white blood cell count and C-reactive protein be included in laboratory tests for early monitoring of infection.15 In addition to peripheral capillary oxygen saturation (SpO2), a lymphocyte count below 1100/μl and an elevated CRP level were used for early patient triage. In combination with clinical signs, these parameters helped to differentiate patients requiring hospitalization from those who could stay at home with self-isolation. Therefore, hematology instruments that combine CRP and CBC analysis from the same sample made sense for rapid diagnosis and were preferred by many clinics.
CRP is one of the inflammatory markers that can effectively assess disease severity. High levels of CRP are associated with the development of severe disease and are correlated with lung lesions in the early stages of Covid-19.16,17 Elevated CRP has been shown to be associated with a poor prognosis in Covid-19-positive patients and is therefore used as a marker to monitor disease progression.18
In addition to the applications described above, the analysis of CRP together with a complete blood count plays an important role in many other diagnostic situations. For example, it is used in the diagnosis of appendicitis, as CRP has the highest diagnostic accuracy in complicated cases. The diagnosis of appendicitis should not be made only based on clinical examination alone, and more specific and systemic markers of inflammation are needed. The combination of CRP and WBC may improve the diagnosis. The combined use of cut-off values for WBC (≥13100/μL) and CRP (≥1.17 mg/L) gives a higher sensitivity for the diagnosis of complicated appendicitis.19
As a growing number of experimental studies suggest a link between inflammation and cancer, several observational studies have been conducted to investigate the association between inflammatory markers, such as CRP and white blood cells, and an increased risk of cancer. A Swedish study involving more than 100,000 patients provides further evidence of an association between elevated CRP and leukocyte levels and overall cancer risk.20 Furthermore, CRP and leukocyte count may be dual prognostic predictors in solid tumors and hematological malignancies.21
Diagnostic testing for autoimmune diseases is another area where CBC and inflammatory markers such as CRP are needed. Because autoimmune diseases can affect multiple organs and cause highly variable signs and symptoms that can change in severity over time, recognizing and diagnosing autoimmune diseases can be difficult. Blood tests that indicate the presence of inflammation are usually used to diagnose an autoimmune disease. A complete blood count (CBC) may show characteristic findings such as normocytic, normochromic anemia, which indicates the chronicity or severity of the disease, and an increased or decreased platelet and/or white blood cell count. In combination with CRP, more detailed information about an ongoing inflammation can be obtained.22
This summary shows that the combination of CRP and CBC markers is necessary and beneficial in the diagnosis of many different diseases. However, the traditional workflow for analyzing these markers on different diagnostic platforms is not straightforward and it usually takes time before a treatment decision can be made.
HumaCount 5DCRP –
the ideal 2-in-1 solution for 5-part Diff and CRP from one drop of blood
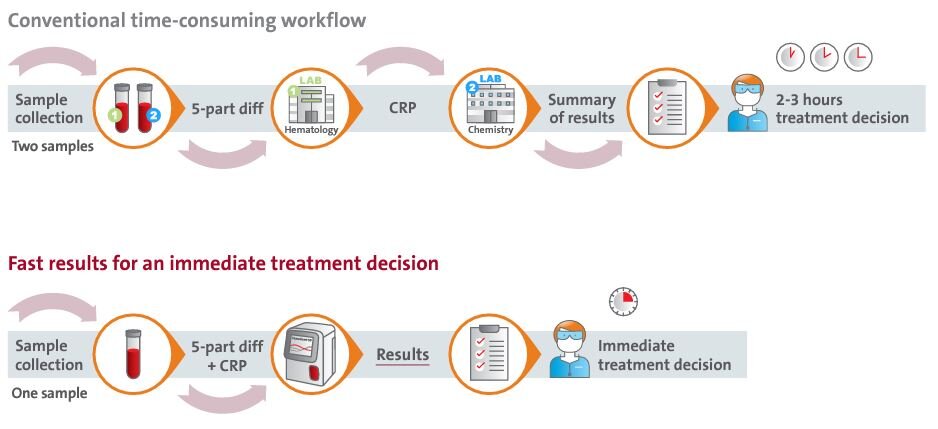
The conventional workflow for testing CRP and CBC is quite time-consuming. It requires two blood samples to be taken from the patient, a whole blood sample for CBC and a serum or plasma sample for CRP.
The detection of CRP using a clinical chemistry analyzer requires several steps. First, the samples must be collected for batch analysis, then they must be prepared by centrifugation, placed on the analyzer, and finally the results of the hematology and CRP tests must be combined. It can take several hours before the doctor can make a treatment decision.
Instead, the HumaCount 5DCRP offers an optimized workflow to combine CRP and CBC analysis from a single blood sample. The system provides rapid results in just 1.5 minutes for timely diagnosis and treatment planning. This increases efficiency and saves costs by eliminating the need for additional tests. It is particularly useful for differentiating between bacterial and viral infections and can help combat the global health problem of antimicrobial resistance by avoiding unnecessary antibiotic prescriptions.

Optimized workflow with HumaCount 5DCRP
Improved efficiency and quality of clinical examination
The combination of CBC and CRP testing provides information of great clinical value, enabling faster and more accurate medical decisions to reduce hospitalization time and patient costs. Patients benefit from easy and painless blood collection using capillary venipuncture.
The OptimalCount technology, which requires only 20μl of capillary blood, ensures correct dilution ratios by auto-diluent dispensing and performs a count of ~3000 cells. This combination of factors results in a high level of accuracy typically only achieved with venous samples.
Pediatric clinics and maternity wards will benefit greatly from this direct capillary blood method. It can also be useful for any patient with fragile veins, e.g., the elderly, patients undergoing chemotherapy or those with a fear of needles. Doctors can take advantage of improved diagnostics to distinguish between viral and bacterial infections. Often, patients with a respiratory infection expect the doctor to prescribe antibiotics – even when the illness could be caused by a viral infection where antibiotics are useless. With the HumaCount 5DCRP, the combination of CRP and CBC provides a clear diagnosis, and the results can also be used to explain to the patient why antibiotics may not be indicated. With a small footprint and no need for an external computer, the unit can be installed in a doctor's office where space may be limited.
The HumaCount 5DCRP could also be a useful addition on hospital wards, close to the patient, to quickly monitor the patient's health status without having to send a sample to the central laboratory and wait for the results. The same applies to situations where quick decisions are extremely important, such as in the emergency room or intensive care unit.
Conclusion and outlook
In summary, the HumaCount 5DCRP with its unique combination of a complete blood count together with CRP is a useful addition to a variety of diagnostic applications and many different types of users can benefit from the system. It is the ideal system for rapid diagnosis, but also for acute and chronic disease monitoring, infection monitoring, antibiotic efficacy, and patient treatment monitoring.
References
- www.testing.com/tests/complete-blood-count-cbc/ Accessed September 19, 2023
- https://www.testing.com/tests/c-reactive-protein-crp/ Accessed September 19, 2023
- Thomas, L. C-reaktives Protein (CRP) In: Prof. Dr. Lothar Thomas, Kirschbaumweg 8, 60489 Frankfurt (ed.) Labor und Diagnose 2020. Chapter 19.4. Accessed September 19, 2023. https://www.labor-und-diagnose-2020.de
- De Sutter A, Lemiengre M, Van Maele G, van Driel M, De Meyere M, Christiaens T, De Maeseneer J. Predicting prognosis and effect of antibiotic treatment in rhinosinusitis. Ann Fam Med. 2006 Nov-Dec;4(6):486-93. doi: 10.1370/afm.600. PMID: 17148625; PMCID: PMC1687172.
- Hopstaken RM, Stobberingh EE, Knottnerus JA, Muris JW, Nelemans P, Rinkens PE, Dinant GJ. Clinical items not helpful in differentiating viral from bacterial lower respiratory tract infections in general practice. J Clin Epidemiol. 2005 Feb;58(2):175-83. doi: 10.1016/j.jclinepi.2004.08.004. PMID: 15680752.
- Macfarlane J, Holmes W, Gard P, Macfarlane R, Rose D, Weston V, Leinonen M, Saikku P, Myint S. Prospective study of the incidence, aetiology and outcome of adult lower respiratory tract illness in the community. Thorax. 2001 Feb;56(2):109-14. doi: 10.1136/thorax.56.2.109. PMID: 11209098; PMCID: PMC1746009.
- https://www.cdc.gov/patientsafety/features/be-antibiotics-aware.html Accessed September 19, 2023
- https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance Accessed September 19, 2023
- Caldas JP, Marba ST, Blotta MH, Calil R, Morais SS, Oliveira RT. Accuracy of white blood cell count, C-reactive protein, interleukin-6 and tumor necrosis factor alpha for diagnosing late neonatal sepsis. J Pediatr (Rio J). 2008 Nov-Dec;84(6):536-42. English, Portuguese. doi: 10.2223/JPED.1838. PMID: 19060982.
- Escadafal C, Incardona S, Fernandez-Carballo BL, Dittrich S. The good and the bad: using C reactive protein to distinguish bacterial from non-bacterial infection among febrile patients in low-resource settings. BMJ Glob Health. 2020 May;5(5):e002396. doi: 10.1136/bmjgh-2020-002396. PMID: 32467355; PMCID: PMC7259834.
- Wilson M. Fever in returned travelers. In: Keystone J, Kozarsky PE, Freedman DO, editors. Travel medicine. 2nd. Philadelphia, PA: Elsevier; 2008. pp. 513–521.
- Cooper EC, Ratnam I, Mohebbi M, Leder K. Laboratory features of common causes of fever in returned travelers. J Travel Med. 2014 Jul-Aug;21(4):235-9. doi: 10.1111/jtm.12122. Epub 2014 Apr 22. PMID: 24754384.
- Wilson M. Fever in returned travelers. In: Keystone J, Kozarsky PE, Freedman DO, editors. Travel medicine. 2nd. Philadelphia, PA: Elsevier; 2008. pp. 513–521
- Nishimura J, Dharap P, Raimbault S. The utility of basic blood counts, WBC histogram and C-reactive protein in detecting malaria. BMC Infect Dis. 2021 Sep 26;21(1):1006. doi: 10.1186/s12879-021-06704-5. PMID: 34565334; PMCID: PMC8474782.
- Zhang J, Zhou L, Yang Y, Peng W, Wang W, Chen X. Therapeutic and triage strategies for 2019 novel coronavirus disease in fever clinics. Lancet Respir Med. 2020 Mar;8(3):e11-e12. doi: 10.1016/S2213-2600(20)30071-0. Epub 2020 Feb 13. PMID: 32061335; PMCID: PMC7159020.
- Wang L. C-reactive protein levels in the early stage of COVID-19. Med Mal Infect. 2020 Jun;50(4):332-334. doi: 10.1016/j.medmal.2020.03.007. Epub 2020 Mar 31. PMID: 32243911; PMCID: PMC7146693
- Liu F, Li L, Xu M, Wu J, Luo D, Zhu Y, Li B, Song X, Zhou X. Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J Clin Virol. 2020 Jun;127:104370. doi: 10.1016/j.jcv.2020.104370. Epub 2020 Apr 14. PMID: 32344321; PMCID: PMC7194648.
- Malik P, Patel U, Mehta D, Patel N, Kelkar R, Akrmah M, Gabrilove JL, Sacks H. Biomarkers and outcomes of COVID-19 hospitalisations: systematic review and meta-analysis. BMJ Evid Based Med. 2021 Jun;26(3):107-108. doi: 10.1136/bmjebm-2020-111536. Epub 2020 Sep 15. PMID: 32934000; PMCID: PMC7493072
- Buyukbese Sarsu S, Sarac F. Diagnostic Value of White Blood Cell and C-Reactive Protein in Pediatric Appendicitis. Biomed Res Int. 2016;2016:6508619. doi: 10.1155/2016/6508619. Epub 2016 May 4. PMID: 27274988; PMCID: PMC4870336.
- Van Hemelrijck M, Holmberg L, Garmo H, Hammar N, Walldius G, Binda E, Lambe M, Jungner I. Association between levels of C-reactive protein and leukocytes and cancer: three repeated measurements in the Swedish AMORIS study. Cancer Epidemiol Biomarkers Prev. 2011 Mar;20(3):428-37. doi: 10.1158/1055-9965.EPI-10-1190. Epub 2011 Feb 4. PMID: 21297038; PMCID: PMC3078551
- Bruserud Ø, Aarstad HH, Tvedt THA. Combined C-Reactive Protein and Novel Inflammatory Parameters as a Predictor in Cancer-What Can We Learn from the Hematological Experience? Cancers (Basel). 2020 Jul 19;12(7):1966. doi: 10.3390/cancers12071966. PMID: 32707721; PMCID: PMC7409204
- Castro C, Gourley M. Diagnostic testing and interpretation of tests for autoimmunity. J Allergy Clin Immunol. 2010 Feb;125(2 Suppl 2):S238-47. doi: 10.1016/j.jaci.2009.09.041. Epub 2010 Jan 12. PMID: 20061009; PMCID: PMC2832720.